Oral Microbiome, Dysbiosis, and the Paradigm of Integrative Dental Medicine
Reframing Oral Health Beyond the Conventional Paradigm
For decades, dentistry has been dominated by a mechanistic orientation, emphasizing mechanical plaque removal, caries prevention through fluoride delivery, and gingival stabilization via antiseptic rinses and clinical scaling. While these interventions retain clinical merit, they inadequately address the ecological, immunological, and systemic complexity of the oral cavity. Advances in oral microbial ecology, mucosal immunology, neuroendocrine biology, and systems medicine now underscore a more profound reality: the oral cavity is not merely a localized anatomical site susceptible to caries and periodontal disease, but rather a dynamic microbial–immune interface whose balance or disruption reverberates across the human organism. Central to this reconceptualization is the oral microbiome—a polymicrobial consortium comprising bacteria, archaea, fungi, protozoa, and viruses—whose collective genomic and metabolic activity exerts influence over oral health, immune surveillance, cardiovascular homeostasis, metabolic integrity, and neurocognitive resilience.
Perturbations in this ecosystem, termed oral dysbiosis, arise from dietary hyper-refinement (particularly excessive sucrose intake), antibiotic and pharmaceutical exposures, environmental toxins, indiscriminate use of antimicrobial rinses, salivary hypofunction, and psychosocial stressors. Dysbiosis manifests clinically as gingivitis, periodontitis, dental caries, enamel demineralization, and halitosis, yet its consequences extend beyond the oral environment. Robust evidence now links oral microbial imbalance with atherosclerotic burden, insulin resistance, adverse pregnancy outcomes, autoimmune exacerbations, and neurodegenerative trajectories, positioning oral health as a sentinel domain of systemic wellness. As dental scholar Dr. S. Choudhury affirms, “The oral microbiome must be reconceived not as a peripheral adjunct to health, but as a regulatory axis that modulates multisystemic resilience or vulnerability.”



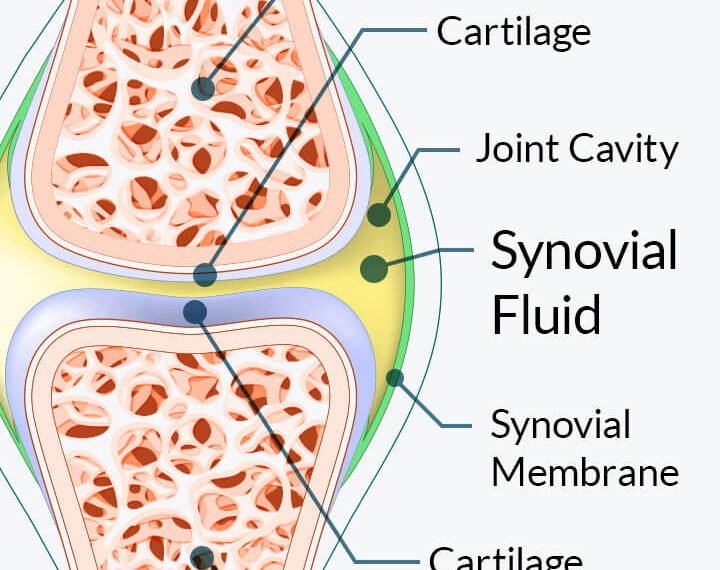
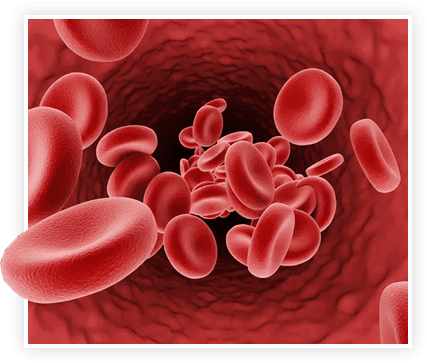
Mechanistic Axes of Oral–Systemic Crosstalk
The interconnections between oral microbial disequilibrium and systemic pathology operate through several interdependent pathways:
- Inflammatory signaling cascades: Dysbiotic microbiota activate gingival and periodontal inflammation, yielding systemic dissemination of pro-inflammatory cytokines, chemokines, and proteases.
- Microbial translocation: Pathogenic taxa such as Porphyromonas gingivalis and Fusobacterium nucleatum penetrate epithelial barriers and infiltrate vascular and organ-specific niches.
- Endotoxin burden: Gram-negative lipopolysaccharides (LPS) amplify oxidative stress, endothelial dysfunction, and vascular remodeling.
- Salivary defense impairment: Saliva, enriched with antimicrobial peptides, secretory immunoglobulins, enzymes, and electrolytes, functions as a biofluid of systemic immunological priming; dysbiosis compromises its regulatory potential.
Together, these mechanisms establish the oral cavity as a pathophysiological gateway to chronic inflammatory, metabolic, and neurodegenerative disease.
Lorem ipsum dolor sit amet, consectetur adipiscing elit. Ut elit tellus, luctus nec ullamcorper mattis, pulvinar dapibus leo.

ProDentim: A Microbiome-Oriented Therapeutic Innovation
ProDentim epitomizes a next-generation synbiotic intervention, designed not to suppress microbial activity indiscriminately but to recalibrate oral ecology, strengthen mucosal defenses, and optimize salivary physiology. Unlike fluoride or antiseptic regimens that risk ecological disruption, ProDentim is constructed upon a systems-oriented architecture, employing probiotics, prebiotics, phytochemical modulators, and micronutrients specifically curated for oral bioactivity.
Bioactive Components and Functional Interactions
Lactobacillus reuteri & Lactobacillus paracasei: Suppress pathogenic overgrowth, stabilize periodontal architecture, and attenuate biofilm virulence.
Bifidobacterium lactis BL-04: Supports epithelial immune resilience while contributing to systemic microbial harmony.
Inulin (prebiotic fiber): Provides substrate for commensal proliferation, enhancing ecological robustness.
Malic Acid (natural strawberry derivative): Stimulates salivary gland secretion, counteracts xerostomia, and facilitates enamel remineralization.
Spearmint polyphenolic compounds: Impart antioxidative, anti-inflammatory, and antimicrobial protection while augmenting sensory freshness.
Collectively, these constituents orchestrate a polyfunctional bioactive matrix, addressing both symptomatic domains (halitosis, gingival irritation) and foundational ecological resilience (salivary defense, enamel mineralization, systemic anti-inflammatory modulation).
Translational Evidence and Clinical Correlates
Emerging data from oral probiotic research demonstrate:
Periodontal benefits: Reduction in plaque scores, bleeding indices, and inflammatory biomarkers.
Microbial recalibration: Transition toward commensal-dominated ecological states.
Systemic biomarkers: Declines in C-reactive protein and circulating cytokines indicative of systemic inflammation.
Patient-reported measures: Enhanced freshness of breath, reduced sensitivity, and improved oral comfort.
Manufacturing Integrity and Clinical Assurance
ProDentim is formulated within FDA-inspected, GMP-certified facilities, ensuring uncompromising standards of purity, potency, and reproducibility. The composition is non-GMO, allergen-sensitive, and free from unnecessary synthetic excipients, rendering it accessible across diverse populations. Its 60-day satisfaction assurance reflects both consumer confidence and manufacturing accountability.
Conclusion: Toward an Integrative, Microbiome-Centered Dentistry
The oral microbiome must be regarded as a systemic regulator, intimately linked with cardiovascular, metabolic, immunological, and neurological domains. Oral dysbiosis propagates a cascade of systemic dysregulation, affirming the inadequacy of hygiene-centered frameworks. By embracing a microbiome-focused and integrative paradigm, ProDentim represents a translationally robust innovation bridging dentistry, microbiology, and systems medicine.
For those seeking a strategy beyond symptomatic palliation—one oriented toward sustained oral and systemic resilience—ProDentim emerges as an evidence-aligned therapeutic model at the forefront of integrative dental medicine.